[ad_1]
This opinion piece, written by Dr. Brett Montgomery of UWA Medical School, was published in The conversation on Friday July 2, 2021.
It’s been a crazy week for public messages about the AstraZeneca COVID-19 vaccine – confusing both for the public and for GPs like me.
Just over two weeks ago, the Australian Technical Advisory Group on Immunization (ATAGI) reported that the AstraZeneca vaccine is now only preferred for people over 60 years of age. The Pfizer vaccine has been promoted in those under the age of 60, but it is not yet widely available.
Prime Minister Scott Morrison sparked controversy on Monday, saying ATAGI advice did not ban the vaccine among younger people. He invited those under 60 to discuss it with their GP. This has been reported as a “massive change” in the immunization schedule.
His comments were reprimanded by health officials and prime ministers.
Meanwhile, Health Minister Greg Hunt explained that there had been “no change” in the medical opinion.
For many, these disagreements were confusing.
Hunt is right, however: ATAGI’s advice has remained the same since mid-June. The advice is careful and nuanced:
The AstraZeneca COVID-19 vaccine can be used in adults under the age of 60 for whom Comirnaty [Pfizer] is not available, the benefits are likely to outweigh the risks to that person, and the person has made an informed decision based on an understanding of the risks and benefits.
Let’s dig into the intricacies of this sentence and try to shed some light rather than heat on the problem.
Three principles for decision making
The ATAGI sentence above contains three principles, all of which should be true if AstraZeneca vaccine is to be used in a person under 60 years of age.
First, the Pfizer vaccine is not expected to be available. This is the case with a lot of people right now. For the record, I was told about waits of about three months for the Pfizer, if you can get an appointment. An increase in availability is promised, but not before October.
Second, the benefits of the AstraZeneca vaccine are expected to outweigh the risks. This is difficult, as the risks and benefits can be difficult to estimate.
The major (and well-known) risk of AstraZeneca vaccine is an unusual coagulation syndrome, which is rare, treatable, but sometimes fatal.
The benefits include prevention of COVID and its consequences, including hospitalization and death.
The balance between risks and benefits depends on the person’s risk of being exposed to COVID (which may vary depending on travel or occupation) and their risk of poor outcomes (such as death) in the event of COVID .
Age seems to be the biggest risk factor for these terrible consequences, but other conditions also seem to be important, including heart disease, lung disease, high blood pressure, diabetes and cancer. (Although people under the age of 60 with these conditions are eligible for Pfizer, they can currently wait.)
The risk of exposure to the virus greatly depends on how much COVID is present in our community. The less there is, the less likely you are to catch it. But that can change quickly and unpredictably, adding difficulty to decisions.
The third, the person receiving the vaccine must give informed consent based on an understanding of these risks and benefits.
Informed consent
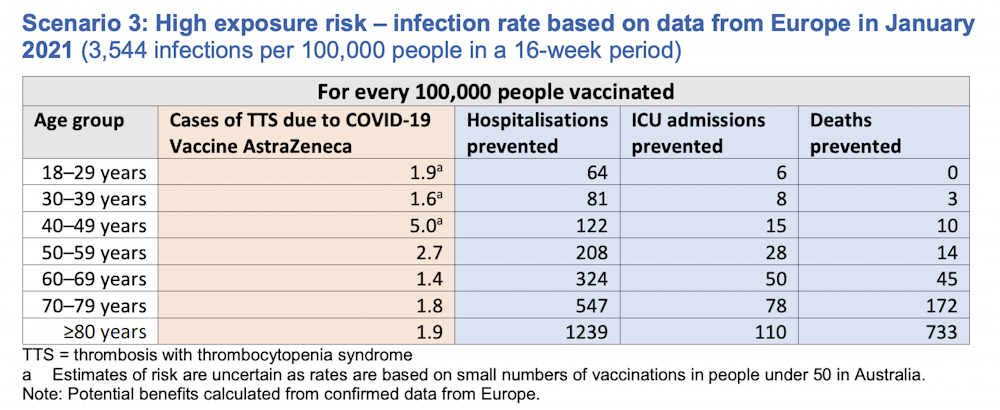
Practical decision aids help visualize some of these risks, but not all. For example, this figure shows the trade-off between risks and benefits during a relatively mild outbreak, equivalent to the first wave of COVID in Australia.
In this context, the benefits of vaccination clearly do not outweigh the risks until people are over 60 years of age. This is why ATAGI used 60 years as the age threshold for the use of the AstraZeneca vaccine.
But if we had a serious epidemic, like in Europe last winter, the benefits of the vaccine would easily outweigh the risks, even in people aged 30 and over.
Individual decisions
These graphs are useful for thinking about how age and disease prevalence affects decisions. But they don’t include all of the relevant facts. For this, a discussion with a GP could be helpful – ideally a GP who knows you well.
ATAGI Co-Chair Christopher Blyth recently clarified that the AstraZeneca vaccine should only be used within 60 years under “pressing” circumstances.
I can imagine such circumstances. For example, consider a 59-year-old man with diabetes and heart disease who plans to travel to a country with high COVID cases. Here I would feel confident that the benefits outweigh the risks.
However, imagine a 25-year-old with no underlying medical condition, not traveling and not working in a high-risk profession. Compared to the previous example, the risks are similar, but the benefits are lower. It would be difficult to convince me that the benefits would outweigh the damage here – at least not while our COVID case count remains low.
However, our number of cases is unlikely to stay low forever and if we wait for a major outbreak before vaccinating, immunity may come too late.
These are heavy decisions, full of ethical tensions. I want to respect my patient’s autonomy – and there’s a part of me that thinks I should be able to vaccinate anyone if they are informed and want the vaccine. After all, many people take other, bigger risks elsewhere in their lives.
And it is admirable that many young Australians who seek to be vaccinated do so not only for themselves, but also to protect their community. But balanced with this, we must try to minimize the damage.
Under 60 and still looking for a vaccine?
If you want to get the vaccine and you are under 60 and Pfizer is not available, you can talk to your GP, especially if your situation puts you at particular risk.
I think it is better to do this during a special consultation rather than squeezing it into a vaccination clinic time slot. Since our vaccines come in multi-dose vials, most practices run fairly rapid-fire vaccination clinics, allowing each person only a few minutes. Such clinics are useful for uncontroversial vaccine decisions in people over the age of 60, but might not allow enough time for complex decisions with younger people.
By working with your GP, I hope that you will feel that you can make the decision that is best suited to your situation and your values.
[ad_2]